In Vitro Fertilization Services
Natural or unassisted conception is when an egg and sperm are fertilized inside a woman’s body. If the fertilized egg attaches to the lining of the womb and continues to grow, a baby is born about 9 months later. When natural conception is not possible and less invasive fertility techniques have been unsuccessful, in vitro fertilization (IVF) is the next step to try to achieve pregnancy.
What Is IVF?
IVF is a form of assisted reproductive technology (ART) during which an egg is fertilized with sperm outside the body in a specialized laboratory setting. If fertilization is successful and results in a good quality embryo, the embryo is transferred into the uterus with the intent of implantation and pregnancy. Depending on individual needs, the egg and sperm used could be from the intended parent(s) or from an egg or sperm donor.
Back to Top
IVF Process
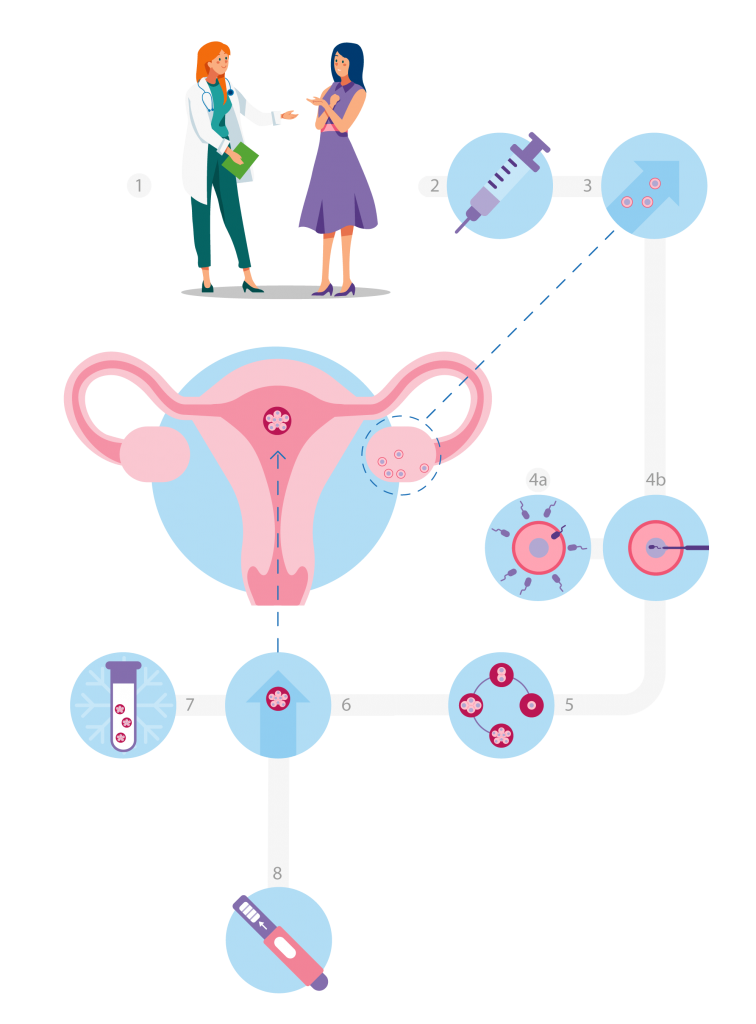
Step 1: Physician Consult

- A consult will be scheduled with a Reproductive Endocrinologist and Infertility (REI) physician to discuss medical history, family goals, and options going forward.
Step 2: Ovarian Stimulation
- Fertility medications will be prescribed to boost egg production in the ovaries.
- Over the next 10 to 12 days, there will be regular pelvic ultrasounds to examine the developing follicles and blood tests to check hormone levels.
- When the time is right, a hormone trigger is given. Egg retrieval is scheduled approximately 36 hours later.
Step 3: Egg Retrieval
- A minor outpatient surgery, called follicular aspiration, is done at one of the KP Centers for Reproductive Health to retrieve eggs from the woman’s body.
- Using ultrasound guidance, the physician will insert a thin needle through the vagina and into the ovarian follicles. The eggs are drawn out of the follicles with gentle suction.
- Anesthesia is used to minimize discomfort during the procedure. Recovery time is generally one hour, after which patients are typically ready to leave the clinic with an adult’s assistance. There may be some cramping after the procedure.
Step 4: Insemination and Fertilization
- Insemination is the process of bringing sperm and eggs together with the intent of fertilization and embryo development. Sperm is either placed with the eggs to allow for natural insemination (step 4a) or it is injected into the mature eggs via a method called intracytoplasmic sperm injection (ICSI) (step 4b). ICSI is recommended when the chance of natural fertilization is low, when the reason for infertility is unknown, or when genetic testing is planned.
- The combined eggs and sperm are then stored in an environmentally controlled chamber (incubator) to allow for fertilization and growth over the next 5 to 6 days.
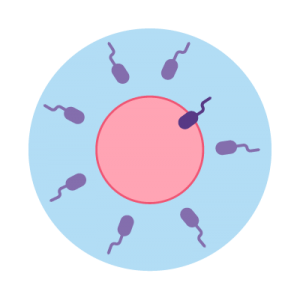
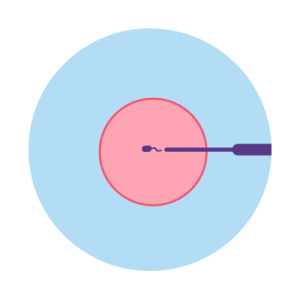
Conventional IVF Insemination
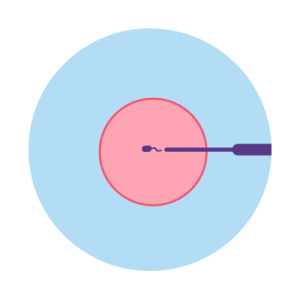
ICSI (Intracytoplasmic Sperm Injection)
Step 5: Embryo Culture
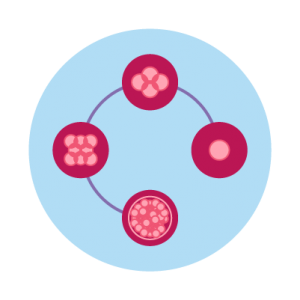
- Over the next 5 to 6 days, the embryos (fertilized eggs) start developing and growing. Those that develop normally are considered “blastocysts” by day 5. On day 5, the embryologists in the lab will assess the growth and quality of each embryo and provide a report of the outcomes.
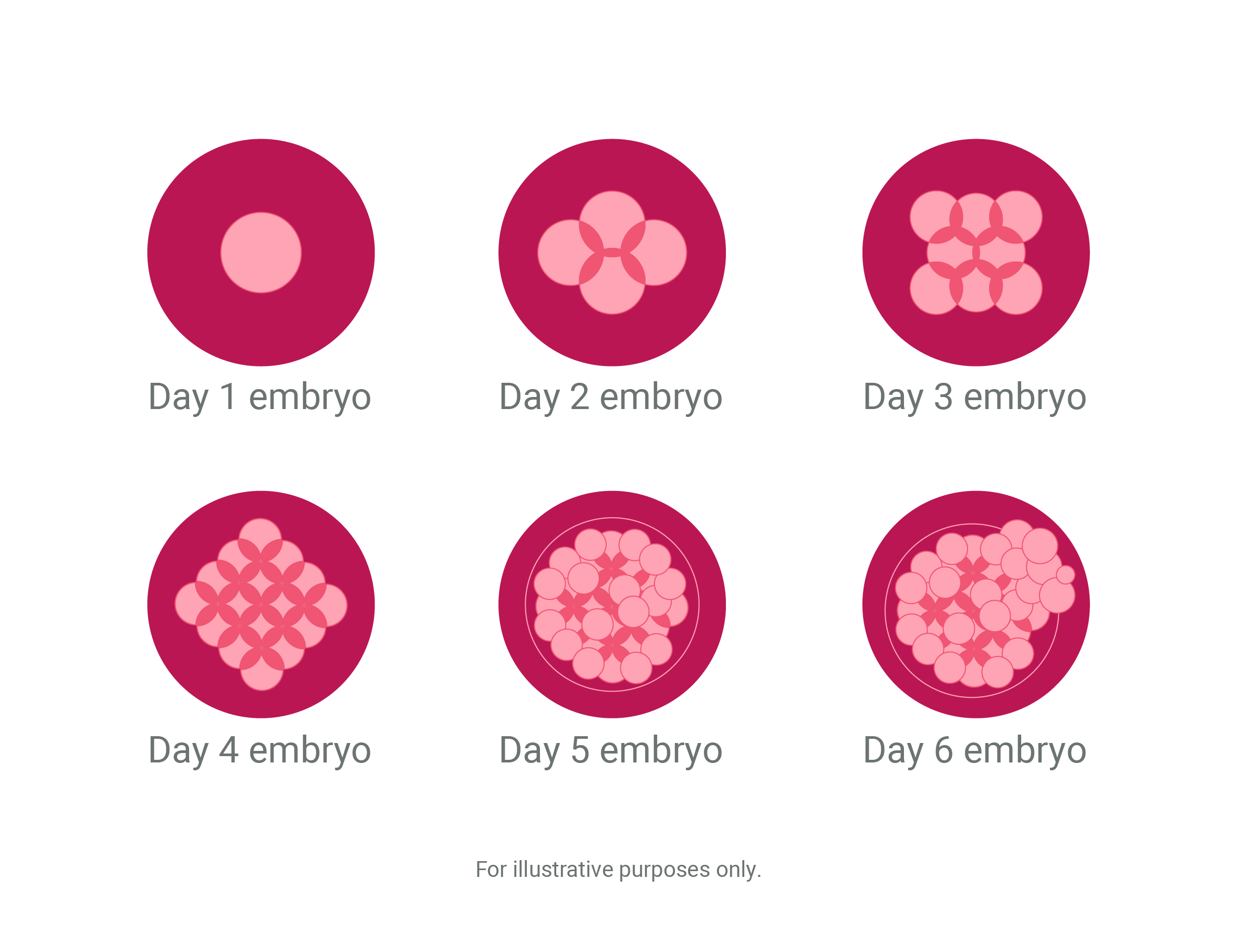
Typical Embryo Development
Pre-Implantation Genetic Testing (Optional)
- Pre-implantation genetic testing (PGT) offers information about the embryo(s) beyond the visual assessment, allowing the selection of a genetically normal (euploid) embryo for transfer.
- On day 5 or 6 following fertilization, the blastocysts are graded. Those meeting specific criteria undergo sampling (biopsy) of the trophectoderm (the cells that will eventually form the placenta). These cells are sent to an outside lab for assessment. The biopsied embryos are then frozen and stored. Genetically normal blastocysts will be thawed and transferred at a later time. This type of cycle is called a freeze all and involves a subsequent frozen embryo transfer (FET) once the genetic testing results are available.
Step 6: Embryo Transfer
- The embryo transfer is also an outpatient procedure done in the KP Centers for Reproductive Health. Sedation is typically not required.
- A thin tube (catheter) containing the embryo for transfer is inserted into the uterus through the cervix. If the embryo implants in the uterine lining and grows, pregnancy results.
- For fresh transfers, the embryo is transferred into the uterus on day 5 after egg retrieval and fertilization. Any remaining good quality embryos are frozen for future transfer. For frozen embryo transfers (FET), the previously frozen embryo is thawed and then transferred.
- KP Centers for Reproductive Health follow the American Society of Reproductive Medicine (ASRM) guidelines for number of embryos to transfer.
- In the case of genetically normal embryos, it will always be recommended that patients transfer one embryo at a time.
Step 7: Cryopreservation and Tissue Storage
- Embryos are frozen by a Kaiser Permanente embryologist via a state-of-the-art method called vitrification. This flash freezing process better preserves the tissue.
- The embryos are stored in temperature monitored liquid nitrogen storage containers that are evaluated daily by the embryology staff. Changes to liquid nitrogen levels are also monitored by 24/7 alarms that notify the embryology staff directly.
Step 8: Pregnancy Testing
- Human chorionic gonadotropin (HCG) levels are measured via a blood test to confirm pregnancy approximately 9 to 11 days after embryo transfer. A second HCG blood test is done 2 to 4 days later. The trend between the first and second tests is used to determine the viability of the pregnancy.
KP IVF Cycle Types & Services
Fresh Cycle
In a fresh cycle, eggs are retrieved, fertilized, and assessed over 5 to 6 days. The highest quality embryo is selected and transferred back to the uterus on day 5. If remaining high quality embryos are available, they will be frozen for future use.
Freeze All Cycle
A freeze all cycle foregoes a fresh cycle transfer. Good quality embryos are cryopreserved (frozen) by a process called vitrification and stored until the patient is ready for a transfer. A freeze all cycle may be planned or unplanned for reasons including genetic testing, physician/patient preference, patient health considerations, etc.
Frozen Embryo Transfer (FET)
FET cycles utilize embryos that were previously frozen; they are thawed and transferred to the uterus.
Endometrial Receptivity Analysis (ERA)
An ERA can be done prior to a Frozen Embryo Transfer (FET) to determine the optimal time to transfer an embryo to the uterus. ERA cycles mimic an FET cycle; however, instead of transferring an embryo, a small sample of endometrial tissue is taken from the uterus and sent to a genetics lab for assessment and information on timing an embryo transfer.
Intracytoplasmic Sperm Injection (ICSI)
ICSI uses micro-manipulative techniques to inject a single sperm directly into an egg. Only mature eggs ready for fertilization are selected for this process. Most often, ICSI is used in cases of known or suspected male factor infertility, or in cases of previously demonstrated poor fertilization rates. ICSI is also recommended in cases where pre-genetic implantation testing is planned.
Assisted Hatching (AH)
Assisted hatching uses micro-laser technology to create a small slit or opening in the protective coating surrounding an embryo, making it easier for the embryo to “hatch” before being implanted into the woman’s uterus. Assisted hatching may increase the chance of implantation, especially in older women.
Preimplantation Genetic Testing for Aneuploidies (PGT-A)
PGT-A screening examines the number of chromosomes in an embryo. Aneuploid embryos have an abnormal number of chromosomes, which can cause miscarriage or lead to genetic conditions in the child. Euploid or chromosomally normal embryos increase the likelihood of IVF being successful and resulting in pregnancy and live birth.
Preimplantation Genetic Testing for Monogenic / Single Gene Disorders (PGT-M)
PGT-M is used to test embryos for the potential for specific genetic disorders to which the couple may be predisposed. PGT-M is used to:
- Prevent the passing of a genetic disease to the offspring particularly if patients are at risk of passing on inherited genetic diseases such as cystic fibrosis and muscular dystrophy.
- Avoid the transfer of embryos that may be affected by a certain genetic condition.
Embryo Cryopreservation and Storage
Cryopreservation involves freezing and storing good quality embryos during an IVF cycle. These frozen embryos are available for use in a later frozen embryo transfer cycle. Kaiser Permanente offers 6 months of courtesy onsite tissue storage at the Centers for Reproductive Health.* At the end of this courtesy period, the tissue is shipped for long term tissue storage to our designated third-party facility, where annual storage fees are billed directly to patient unless an insurance benefit applies.
*Courtesy storage only applies to samples kept at Kaiser Permanente for the first 6 months of storage. Certain cases require that tissue be sent to our third-party storage facility immediately. In these cases, short-term courtesy storage does not apply.
Third-Party Cycles
A third-party cycle is an infertility cycle that involves a donated egg or sperm, and/or a gestational carrier (surrogate). These cycles provide a viable option for treating those who otherwise would not be able to conceive and/or carry a pregnancy on their own.
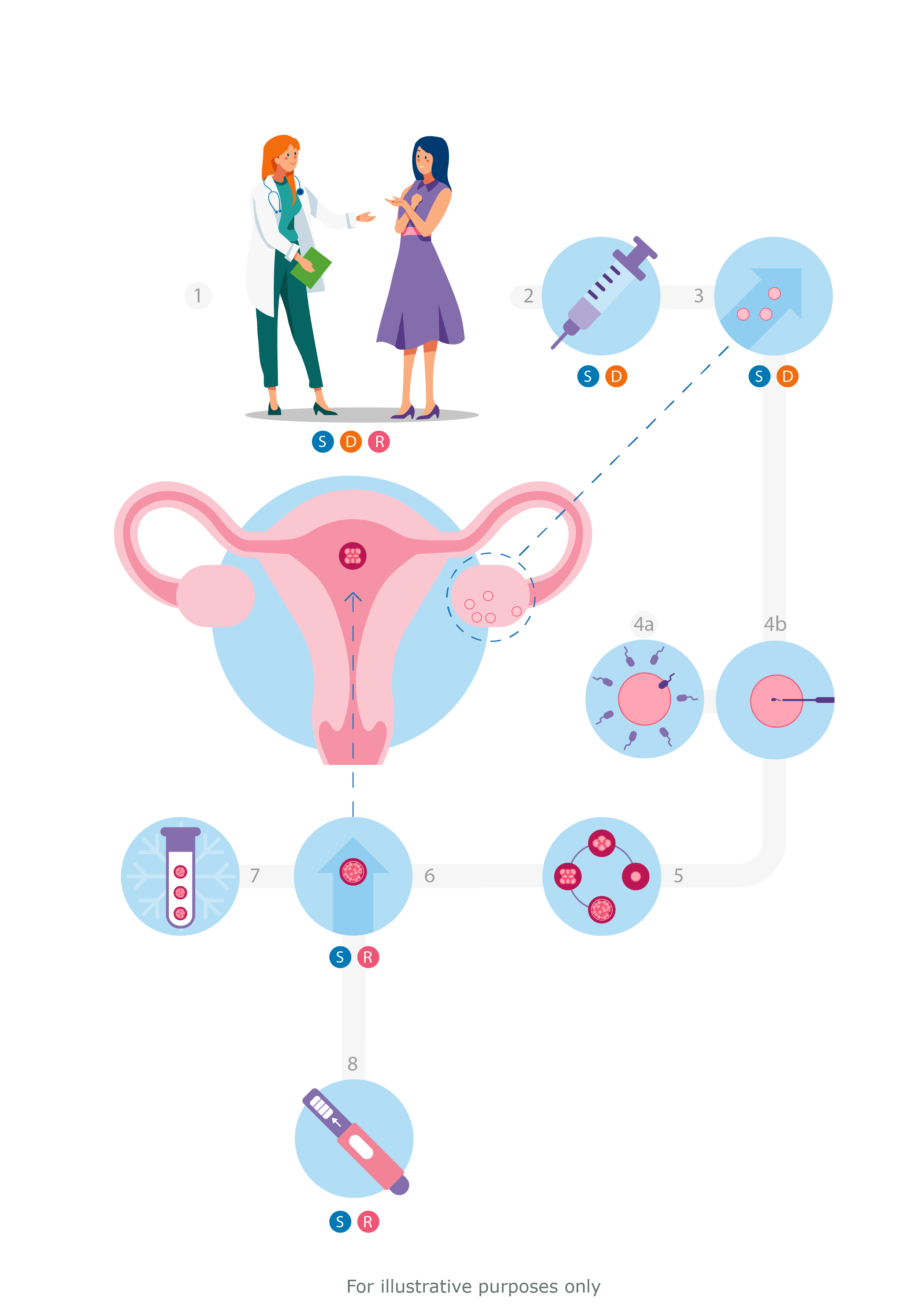
1. Consultation SDR
2. Stimulate ovaries SD
3. Retrieve eggs SD
4. Fertilize eggs
5. Monitor embryo growth
6. Transfer embryo to uterus SR
7. Freeze remaining embryos
8. Test for pregnancy SR
S = Self
D = Donor
R = Recipient
Using Donor Eggs
The IVF process is similar when using an egg donor. The main difference is that the process is split between the egg donor and embryo recipient.
If you and your provider have decided to pursue IVF with donor eggs, the team at the KP Centers for Reproductive Health are here to assist you.
We will help you:
- Understand the donor selection process using an agency or identifying someone independently.
- Coordinate all screening and cycle monitoring for both donor and recipient:
- Complete required screening tests as well as meet with a psychologist.
- Prepare the donor for egg retrieval, including ordering the medication used to stimulate her ovaries. The recipient will take medication to develop her endometrium, the lining of the uterus, for embryo transfer and implantation.
- Coordinate monitoring visits for the donor and recipient. Monitoring visits include blood tests and ultrasounds. The recipient typically has 2 to 3 visits and the donor has approximately 4 to 6. These visits are coordinated on separate days to maintain confidentiality.
Our experienced staff will guide both the donor and recipient through this process. Visit our Donor Cycle FAQ for more information about using an egg donor.
Using Donor Sperm
If you would like to proceed with a sperm donor cycle after speaking with your provider, you should contact an FDA approved cryobank to select donor sperm that meets your needs. The cryobank must have a California Tissue Bank license, which can be validated through the cryobank’s website or by calling them directly.
Intrauterine insemination (IUI) and in vitro fertilization (IVF) are both options when using donor sperm. The process and medications involved are the same as when using partner sperm for IUIs or IVF. Your doctor must review the donor records (e.g., genetic testing results) before you make your final decision on a donor.
Couples who would like to use eggs from one person and donor sperm to create embryos that will then be transferred to the other person will need to undergo IVF.
Using a Gestational Carrier (Surrogate)
The Gestational Carrier Program was established to support families who, due to medical reasons, are unable to carry their own pregnancy. Embryos created through IVF from the intended parents’ eggs or donor eggs and the intended parents’ sperm or donor sperm are transferred to the uterus of a gestational carrier for implantation and intended pregnancy. The gestational carrier will undergo monitoring ultrasounds and will take medications in preparation for embryo transfer.
Identifying a Gestational Carrier
There are two types of gestational carriers:
- Agency gestational carrier. Individuals are recruited and psychologically screened by an agency separate from our clinic. The agency will coordinate all legal contracts, parentage agreements, trust accounts and provide support to all parties.
We will provide you with a referral list of gestational carrier agencies.
- Known gestational carrier. A friend or family member who is willing to be a gestational carrier for you. We encourage the parties involved to seek legal counsel prior to the start of a treatment cycle.
Gestational Carrier Requirements
- Be between the ages of 21 and 40.
- Must have a history of delivering a baby at term. (If only a single term delivery, this child cannot have been given up for adoption.)
- Must be healthy, not overweight, a non-smoker and not have any chronic health problems or have had high risk/complicated pregnancies.
- Must have some type of medical insurance (not Medi-Cal) and have insurance review of their current policy to confirm they have insurance benefits for surrogacy. Some plans exclude surrogacy, in which case, the recipient may be responsible for medical costs during the pregnancy and delivery.
- Must have a physical exam, saline sonogram, mock embryo transfer, hysterosalpingogram and mid-cycle lining check ultrasound.
- Must have infectious disease lab and drug testing done.
- Must take a multiple-choice psychological test and have two face-to-face meetings with a psychologist.
- Surrogate’s partner/spouse will also be required to be tested for infectious diseases and to participate in the psychological consultations.
About 30% of known surrogate candidates do NOT pass all the screening tests or have insurance that provides for surrogacy benefits.
The intended parent(s) will be referred to an attorney specializing in reproductive law to handle the legal contracts and parentage agreements.
Learn More
Visit the following FAQ pages for more information.
